What is homocysteine? And why is it a word that every adult serious about their long-term health needs to know?
We’re all familiar with the “big” risk factors for cardiovascular disease (CVD): high cholesterol, high blood pressure, and smoking. Yet, CVD remains the number one cause of death globally, accounting for a staggering 42% of all deaths in the United States alone.
This suggests that even if you manage your cholesterol, you might be missing a critical part of the puzzle. For decades, researchers have been investigating a “hidden” risk factor—a metabolic by-product that, when elevated, dramatically increases the risk of heart attack and stroke.
That risk factor is homocysteine.
This post is a “mini white paper” that explores the science of this dangerous amino acid. We will answer what is homocysteine, how it attacks your body, and the “Evidence First” nutritional strategy—involving specific B-vitamins and lipotropic factors—that is clinically proven to control it.
🔬 The Science: The “Hidden” Risk Factor in Your Blood
For years, high cholesterol was the primary villain in the story of heart disease. But this never explained the whole story. After all, many people who suffer heart attacks have normal cholesterol levels. This fact has led researchers to investigate other causes.
What is Homocysteine?
Homocysteine is a common amino acid found in your blood. It is a natural by-product of your body’s metabolic processes, specifically the “homocysteine cycle”. In a healthy body, homocysteine is quickly converted into other harmless or useful substances.
The problem begins when this metabolic cycle breaks down.
When this happens, homocysteine is not converted. Instead, it accumulates in the blood to dangerous levels.
The 1966 Discovery: A Link to Damaged Arteries
The first major clue came in 1966 when Dr. Kilmer S. McCully made a landmark observation. He linked high levels of homocysteine to severe blood vessel disease in children with a rare genetic disorder. This sparked decades of research to see if this link held true for the general population.
The Harvard Proof: A 5x Increased Heart Attack Risk
The definitive answer came from the Harvard Physicians’ Health Study. This massive study found that men whose homocysteine levels were in the highest 5% had a five-fold increased risk of a heart attack compared to those in the lowest 5%.
This was a staggering finding, establishing high homocysteine as a powerful, independent risk factor for heart disease.
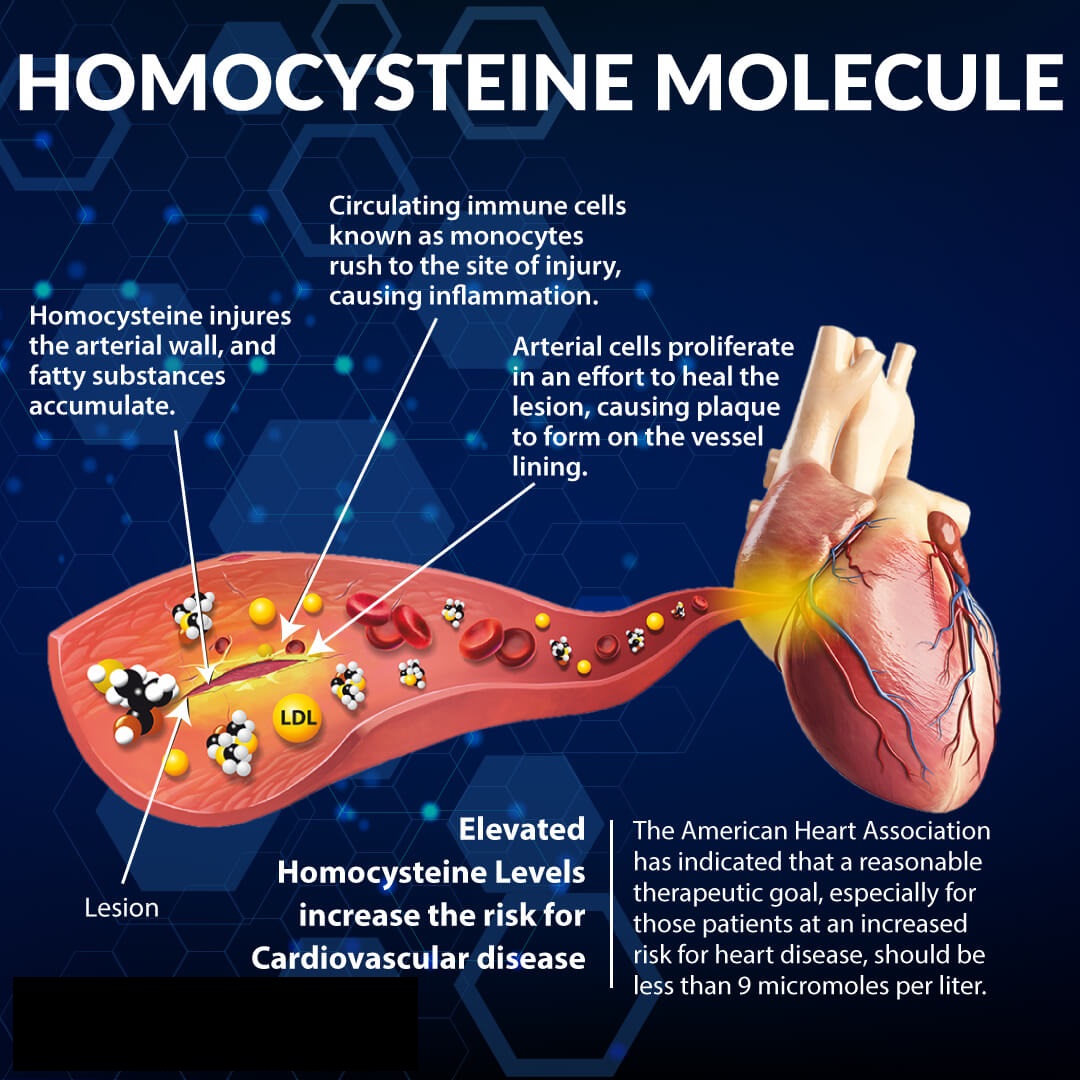
How Homocysteine Attacks the Body
So, what does homocysteine actually do? Unlike cholesterol, which is a problem of accumulation, homocysteine is an attacker.
- It Injures Artery Walls: Scientists believe homocysteine directly injures the delicate endothelial lining of your arteries.
- It Oxidizes LDL Cholesterol: It promotes the oxidation of LDL (“bad”) cholesterol. This “so-called bad cholesterol” is much more dangerous once it is oxidized, as it’s the primary driver of plaque.
- It Leads to Plaque & Clots: This damage and oxidation leads to the formation of atherosclerotic plaques (hardening of the arteries) and thrombosis (clogging of the arteries), which directly lead to heart attacks and strokes.
💡 The Insight: The Metabolic Solution to Homocysteine
The most common reason for dangerously high homocysteine levels is not complex genetics—it’s a simple nutritional deficiency.
Your body has a “Homocysteine Cycle” designed to get rid of this toxic compound. As the diagram shows, it converts homocysteine into other substances. But this entire “engine” requires specific “spark plugs” to run.
The primary nutrients that fuel this conversion are Folic Acid, Vitamin B6, and Vitamin B12.
If you are deficient in these key B-vitamins—a very common situation in a population that doesn’t eat enough fruits and vegetables—this metabolic engine sputters and fails. Homocysteine is not converted, and its levels in your blood begin to rise, increasing your risk for cardiovascular disease every day.
This means that for many people, the risk of high homocysteine is a preventable nutritional problem.
💡 The Insight: What Are Lipotropic Factors? (The “Fat-Moving” Partners)

The B-vitamins are critical, but they are only one half of the cardiovascular health equation. The other half involves lipotropic factors.
“Lipotropic” is a term for compounds that help your body metabolize and transport fats (lipids).
- Choline and Inositol: These two nutrients are the primary lipotropic factors. Their job is to keep fats emulsified (like dish soap breaking up grease in a pan) in your blood.
- Why This Matters: This allows the fats to be mobilized and used for energy, rather than building up as unwanted fat in your liver or on your artery walls.
A third compound, Betaine (also in the homocysteine cycle), is a key helper that not only assists in metabolizing homocysteine but also helps create an environment conducive to Vitamin B12 absorption.
This reveals a complete nutritional strategy:
- You need Lipotropic Factors (Choline, Inositol) to manage the fats in your blood.
- You need B-Vitamins (Folic Acid, B6, B12) to manage the homocysteine in your blood.
🧬 The Proof: Modern Science Confirms the B-Vitamin & Choline Strategy
This nutritional theory is not just based on mid-century research. Modern, high-level clinical trials have continued to prove how powerful this “B-vitamin and lipotropic factor” strategy is—not just for the heart, but for the brain.
The VITACOG Trial: B-Vitamins and Brain Health
The link between homocysteine and cardiovascular disease is well-established. But high homocysteine is also a known risk factor for brain atrophy (shrinkage) and cognitive decline.
The VITACOG trial, a landmark randomized controlled study, investigated this directly.
- The Study: Researchers gave elderly participants with Mild Cognitive Impairment (MCI) and high homocysteine a high-dose supplement of Folic Acid, Vitamin B6, and Vitamin B12.
- The Results: The B-vitamin treatment lowered homocysteine levels by 30%.
- The Astonishing Outcome: In the participants with high baseline homocysteine, the B-vitamin treatment slowed the rate of brain atrophy (shrinkage) by as much as 7-fold in the specific gray matter regions vulnerable to Alzheimer’s disease. The researchers concluded that the B-vitamins lowered homocysteine, which directly led to a decrease in brain atrophy, thereby slowing cognitive decline.
This is profound. The same nutrients that protect your heart are now proven to protect your brain.
The ATTICA Study: Lipotropics and Inflammation
What about the lipotropic factors, choline and betaine? A cross-sectional study of over 3,000 healthy adults (the ATTICA study) investigated their role.
It found that participants consuming the highest levels of choline and betaine had, on average, 22% lower C-reactive protein (CRP) and 26% lower interleukin-6 (IL-6)—two of the body’s primary markers for systemic inflammation.
🧬 The Solution: A Synergistic Complex, Not Isolated Nutrients
The science is clear: a “healthy heart” strategy that only focuses on cholesterol is incomplete. You must also manage homocysteine and lipotropic fats.
But you can’t solve a complex metabolic problem with a simple, isolated B-12 pill. The VITACOG trial didn’t use just one B-vitamin; it used the synergistic team of B6, B12, and Folic Acid. The “Homocysteine Cycle” requires all of them to function.
This is where the NeoLife “Evidence First” philosophy becomes critical.
Why Lipotropic Adjunct is the “Evidence First” Solution
NeoLife’s Lipotropic Adjunct was designed by the Scientific Advisory Board (SAB) to be the complete, synergistic solution to the homocysteine problem. It is not just a B-vitamin pill; it is a complete complex that addresses both sides of cardiovascular health.

Here is the “NeoLife Difference” in every tablet:
- The Complete B-Vitamin Team: It contains the full, proven triad of Folic Acid, Vitamin B6, and Vitamin B12—the exact nutrients shown in the VITACOG trial to lower homocysteine and protect the brain.
- Essential Lipotropic Factors: It delivers Choline and Inositol, the two key nutrients required to help emulsify and mobilize fats, keeping them from building up in the liver and blood vessels.
- Homocysteine Cofactors: It includes Betaine, a key compound that not only participates in the homocysteine cycle but also aids the absorption of Vitamin B12.
- Circulatory Support: It’s finished with Citrus Bioflavonoids, including Hesperidin, which research shows may support circulatory health and healthy blood lipid levels.
🩺 Science Over Shelf Hype
Stop trusting $20 shelf supplements that hide behind flashy claims. The market is flooded with fakes, fillers, and “kitchen sink” formulas with no scientific rationale.
NeoLife is different. We target the real problem. Lipotropic Adjunct is a traceable, science-backed formula, built on 60 years of research. It provides the complete, synergistic team of nutrients clinically proven to support the body’s natural metabolism of homocysteine and fats.
This is not a “pill”—it’s an investment in your cardiovascular and cognitive health.
👉 Explore NeoLife’s Lipotropic Adjunct — a complete, synergistic formula where purity meets performance.
🔗 Further Reading: Keep Learning
- Moving to the (Heart) Beat: A Guide to Your Cardiovascular Health System.
- The Science of Heart Healthy Supplements: A Deeper Look at What Really Works.
- Coenzyme Q10: A Complete Guide to the Science and Benefits
References
- American Heart Association. (1994). Heart and Stroke Facts: 1995 Statistical Supplement.
- Stampfer, M.J., Malinow, M.R., Willett, W.C., et al. (1992). A Prospective Study of Plasma Homocyst(e)ine and Risk of Myocardial Infarction in U.S. Physicians. JAMA, 268:877–881.
- Ueland, P.M., Refsum, H., and Brattström, L. (1992). Plasma Homocysteine and Cardiovascular Disease. In: Francis, R.B., Jr., ed. Atherosclerotic Cardiovascular Disease, Hemostasis, and Endothelial Function. New York: Marcel Dekker, 183–236.
- Selhub, J., Jacques, P.F., Bostom, A.G., et al. (1995). Association Between Plasma Homocysteine and Extracranial Carotid-artery Stenosis. New England Journal of Medicine, 332:286–291.
- Joosten, E., Van Den Berg, A., et al. (1993). Metabolic Evidence that Deficiencies of Vitamin B12 (Cobalamin), Folate and Vitamin B6 Occur Commonly in Elderly People. American Journal of Clinical Nutrition, 58:468–476.
- Selhub, J. and Miller, J.W. (1992). The Pathogenesis of Homocysteinemia: Interruption of the Coordinated Regulation by S-adenosylmethionine of the Remethylation and Transsulfuration of Homocysteine. American Journal of Clinical Nutrition, 55:131–138.
- Olszewski, A.J., Szostak, W.B., Bialkowska, M., et al. (1989). Reduction of Plasma Lipid and Homocysteine Levels by Pyridoxine, Folate, Cobalamin, Choline, Riboflavin, and Troxerutin in Arteriosclerosis. Atherosclerosis, 75:1–6.
- Council for Responsible Nutrition. (1995). CRN News Supplement, April 21, 1995, p.1.
- Ubbink, J.B., Vermaak, W.J., Van der Merwe, A., and Becker, P.J. (1993). Vitamin B12, Vitamin B6 and Folate Nutritional Status in Men with Hyperhomocysteinemia. American Journal of Clinical Nutrition, 57:47–53.
- McCully, K.S. (1994). Chemical Pathology of Homocysteine. III. Cellular Function and Aging. Annals of Clinical Laboratory Science, 24:134–152.
- Olszewski, A.J., and McCully, K.S. (1993). Homocysteine Metabolism and the Oxidative Modification of Proteins and Lipids. Free Radical Biology and Medicine, 14:683–693.
- Cuinod, M., et al. (1989). Homocysteine, Folic Acid and the Prevention of Vascular Disease. Nutr. Rev. 47:247–249.
- Swendseid, M. (1994). Homocysteine, a Putative Pro-oxidant, and the Folate Requirement. Presented at the Western Human Nutrition Research Meeting, San Francisco.
- de Jager, CA., Oulhaj, A., Jacoby, R., et al. (2012). Cognitive and clinical outcomes of homocysteine-lowering B-vitamin treatment in mild cognitive impairment: a randomized controlled trial. International Journal of Geriatric Psychiatry, 27(6), 592-600.
- Detopoulou, P., Panagiotakos, D.B., Antonopoulou, S., et al. (2008). Dietary choline and betaine intakes in relationship to concentrations of inflammatory markers in healthy adults: the ATTICA study. American Journal of Clinical Nutrition, 87(2), 424-430.
- Smith, A.D., Smith, S.M., de Jager, C.A., et al. (2010). Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: A randomized controlled trial. PLoS ONE, 5(9), e12244.
- Douaud, G., Refsum, H., de Jager, C.A., et al. (2013). Preventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatment. PNAS, 110(23), 9523-9528.
- McCully, K.S. (1969). Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. American Journal of Pathology, 56(1), 111-28.